Importance of Intracellular [H+]
The most important [H+] for the body is the intracellular [H+]
Why? Because of its profound effects on metabolism and other cell processes which occur due to the effects of [H+] on the degree of ionisation of intracellular compounds. Specifically:
- Small molecule effect: Intracellular trapping function -due to the ionisation of metabolic intermediates.
- Large molecule effect: Effects on protein function: The function of many intracellular proteins (esp the activities of enzymes) is altered by effects on the ionisation of amino acid residues (esp histidine residues)
In assessment of acid-base disorders, the clinician is always looking from the outside in.
Why? For 2 reasons:
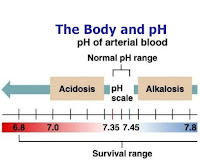
- Ease of sampling: Arterial blood is easy to sample. It is much more difficult to obtain an intracellular sample
- Arterial blood gives results which can be considered a sort of 'average value'. It would be more difficult to find an intracellular sample that could be considered to be 'representative' of all ICF.
The basis of the clinical approach is to use the extracellular results to make inferences about intracellular conditions.
Both carbon dioxide and the fixed acids are produced intracellularly and move down concentration gradients to the ECF. Carbon dioxide crosses cell membranes very easily and it is important to realise that CO2 can move in or out depending on the gradient across the cell membrane.
In diabetic ketoacidosis (DKA), the ketoacids are produced in the liver and not in every cell in the body. The intracellular alkalinising effect of the compensatory hypocapnia that occurs will however affect every cell and not just the hepatocytes. Does this mean that DKA produces an extracellular rise in [H+] but the opposite change in most tissues (excluding the liver) where the net effect is a fall in intracellular [H+] due to the compensatory hypocapnia? Ketoacids can enter most cells and be used as an energy substrate and this would initially cause a fall in intracellular [H+]. Intracellular pH may not be altered much once maximal respiratory compensation has been achieved because of these opposing effects. It is possible that though the maximal respiratory compensation does not fully correct the extracellular acidaemia, it may be sufficient to prevent much change in intracellular pH. This discussion is speculative and has not been fully investigated. The purpose here is merely to show that looking at acid-base disorders from the intracellular viewpoint can lead to ideas which are different from those of the conventional extracellular viewpoint.
The hypothesis of Rahn and coworkers is that the intracellular pH is maintained at about the pH of neutrality (pN) because this is the pH at which metabolite intermediates are all charged and trapped inside the cell. Extracellular pH is higher by 0.5 to 0.6 pH units and this represents about a fourfold gradient favouring the exit of hydrogen ion from the cell. Measurements of intracellular pH in a variety of mammalian skeletal muscle preparations have found pH values mostly in the 6.8 to 7.1 range. Values found in other tissues have sometimes been higher depending on the experimental arrangements. This value is a little higher then the pN (6.8 at 37C) but is still able to effectively trap intermediates within the cell. A further complication is that intracellular pH is not uniform and measurements have been able to give only mean pH values for the whole intracellular compartment. These mean values may be misleading as there may be acidic and basic areas within different cell areas or organelles and it is this local pH which is important.
Because of the powerful effects of intracellular [H+] on metabolism it is useful to consider the processes which attempt to maintain it at a stable value. This assists us in making inferences about intracellular events from an extracellular acid-base sample.
The processes responsible for maintaining a stable intracellular pH are:
- ‘Intracellular buffering’
- Adjustment of arterial pCO2
- Loss of fixed acids from the cell into the extracellular fluid
This term refers to those rapid reversible processes occurring within the intracellular fluid which minimise changes in pH in response to an acid or alkali stress. The term ‘buffering’ is used here in a much broader sense, where it was used to refer to the process of physicochemical buffering alone. Intracellularly, there are other rapid and reversible processes which act to minimise acute changes in intracellular [H+] and which can usefully be considered a form of ‘buffering’. ‘Intracellular buffering’ includes the following processes:
- Physicochemical buffering
- Metabolic buffering
- Organellar buffering
Experiments have shown that these three processes can neutralise over 99.99% of any acid or alkali added acutely to the intracellular fluid! These processes provide rapid but temporary relief from acute intracellular acid-base changes.
Physicochemical buffering
In quantitative terms this is the most important process which resists change in intracellular [H+].
In the intracellular environment, proteins (particularly imidazole of histidine) and phosphates (organic and inorganic) are the most important buffers because they have a pK close to the normal intracellular pH and are present in the highest concentrations. The ICF is responsible for 97 to 99% of the body’s total buffering of respiratory acid-base disorders. The intracellular contribution to buffering is less with metabolic disorders (60% for metabolic acidosis; 30% for metabolic alkalosis) but is still substantial. The bicarbonate system is present intracellularly and is involved in buffering for metabolic acidosis. Intracellular amino acids provide a small amount of the buffering. Free histidine has a pKa of about 6.0 which is lower than the average 6.8 value when it is incorporated into proteins. A small amount of H+ is used up into producing alanine and glutamine.
Metabolic buffering
Metabolic (or biochemical) buffering refers to changes in the metabolism of acids within the cell which tend to oppose changes in [H+].
Changes in intracellular pH affect the activity of enzymes. The net effect of differential changes in enzyme activity in various pathways (including the main glycolytic pathway) is an alteration in the levels of acidic metabolites in such a way that changes in [H+] are minimised. For example, the metabolism of lactate to glucose or to water and CO2(which can readily leave the cell) will effectively remove H+ from intracellular fluid. This is clearly not simply physicochemical buffering. Consider another example: If intracellular pCO2 decreases due to acute hyperventilation, this produces a relative intracellular alkalosis. Changes in enzyme activities result in increased levels of lactate, pyruvate and other acidic intermediates. This occurs quickly, is reversible and tends to minimise the change in intracellular pH. Metabolic buffering can account for a hydrogen ion consumption up to half of that due to the process of physicochemical buffering within the cell.
Organellar buffering
This refers to the acute sequestration in or release of H+ from intracellular organelles in a direction which opposes the change of intracellular pH.
The overall contribution of this process to intracellular buffering is not clear.
The energy released during the electron transfers in the respiratory chain in mitochondria is used to extrude hydrogen ions. The energy is stored as a proton gradient across the inner mitochondrial membrane. When the hydrogen ions re-enter via membrane-bound ATPase, the energy is released and used to produce ATP from ADP. Mitochondria extrude a total of six protons for every oxygen atom that is reduced to water. A rise in cytoplasmic [H+] provides additional H+ which can enter the mitochondria. This will contribute to ATP formation via the inner membrane proton gradient and will buffer changes in cytoplasmic pH.
Lysosomes contain enzymes which have maximal activity at acidic pH. In some experiments, the internal pH of lysosomes increases when extracellular pH increases. This can be interpreted as a mechanism which assists in buffering changes in cytoplasmic pH. The overall significance of this process is not established.
Adjustment of Arterial pCO2
Carbon dioxide is produced in huge quantities by cells: typically 12,000 (basally) to as much as 15,000 to 20,000 mmols/day with typical levels of activity. An efficient system exists for its removal. The arterial pCO2 is of critical importance for intracellular acid-base balance because of both its potential to change rapidly and because of its effectiveness in altering intracellular [H+].
Carbon dioxide crosses cell membranes easily. A change in ventilation affects the arterial pCO2 level and the intracellular pCO2 throughout the body. The compensatory response to a metabolic acid-base disorder is to increase alveolar ventilation and thus decrease arterial pCO2 levels. This changed pCO2 will affect intracellular pH and this effect is rapid. For example an acute metabolic acidosis will be compensated by a fall in pCO2 which will minimise the intracellular effects of the acidosis.
Fixed Acid Extrusion from Cells
Metabolism (an intracellular event) produces excess acid. In the long term, hydrogen ion balance within the cell is dependent on loss of these acids from the cell. The various buffering processes discussed previously are only short-term measures as the acid is not removed from the cell.
Experiments show that cells respond to an acute acid load (eg hypercapnia) by an initial fall in pH (minimised by intracellular buffering discussed above) but that the pH subsequently returns slowly towards normal despite the continued presence of the acid stress. This is due to net acid extrusion from the cell across the cell membrane. This process involves a coupled exchange of ions (H+, HCO3-, Na+ and Cl-) across the membrane. The process does not affect the membrane potential so it must be electroneutral. Various models have been proposed but the relative importance of these in vertebrates has not been fully established. The response of cells to an alkaline load is much less developed and much less studied than the response to an acid load.
The movement of H+ or HCO3- across the membrane is not important in changing [H+] but the movement of strong electrolytes (such as Na+, Cl-, lactate) will alter intracellular [H+]. The important point is that it is the movement of the acid anion out of the cell (rather than hydrogen ion per se) that results in a net loss of fixed acid from the cell. A similar situation applies in the kidney: the emphasis should be on the urinary loss of the acid anions (with the H+ buffered on phosphate of ammonium) rather than hydrogen ion itself. The traditional use of hydrogen ion in explanations must be quantitatively equivalent but does serve to disguise the true nature of the process.
In summary: In experiments where cells are subjected to an acid load, they respond by an increase in the rate of acid extrusion from the cell. This returns intracellular [H+] towards normal. The response is not as rapid as the mechanisms involved in intracellular buffering.
Credit: Kerry Brandis

No comments:
Post a Comment